What is Optical Coherence Tomography?
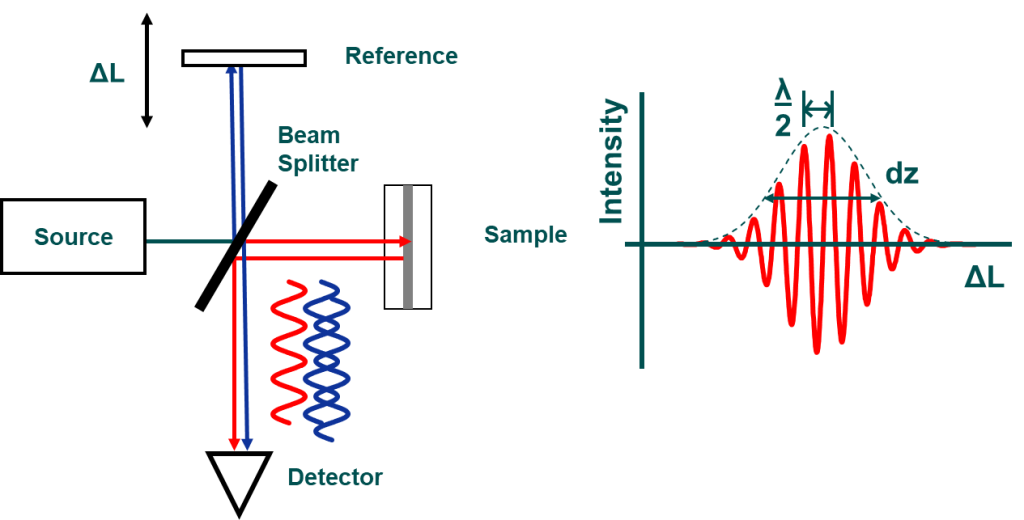
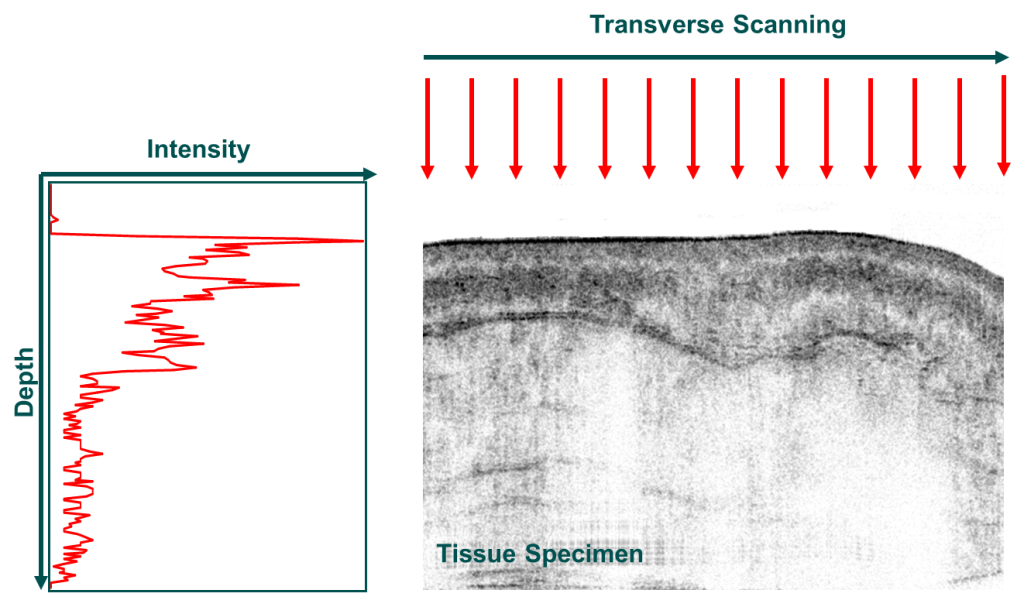
Optical Coherence Tomography (OCT) is an emerging technology used to perform “optical biopsy”, i.e. in situ imaging of tissue microstructure with a resolution approaching that of histology, but without the need for tissue excision and processing. It is analogous to ultrasound, except that it measures intensity of back-reflected light instead of sound. However, it is technologically different than ultrasound since it can achieve resolutions in the order of 1-10 μm at depths of 2-3 mm. Contrast is provided by index of refraction mismatch in tissue. Since light is much faster than sound, interferometric depth localization is used to identify the origin of the back-reflections from within the tissue. Low intensity laser light is split into a reference beam (directed to a mirror) and a sample beam (directed to the tissue). Light is reflected from both and recombines back at a detector creating an interference pattern. Based on the interference pattern the origin of the reflected light is estimated and an image is formed by scanning the laser beam over the tissue. See an OCT presentation here (PDF). For a more scientific description of OCT see reviews here (a, b, c).
See an OCT presentation here
For a more scientific description of OCT see reviews here (Fercher et al 2003, Fujimoto 2003, Podoleanu 2005, Handbook of Biomedical Optics).
Can we “see” more?
Optical Coherence Tomography Research at the ODx Lab
OCT can play a role in early diagnosis of disease and improve patient prognosis since it provides high resolution images (1-15μm) in real-time, non-invasively, and in vivo. However, many cancerous and pre-cancerous changes are in the μm/sub-μm range. These include cell proliferation (5 μm spacing change), nucleus variations (~2-4 μm diameter change) and sub-cellular and sub-nuclear variations (< 1 μm change). Research at the ODx Lab aims to significantly improve the resolution of OCT images and extract additional, normally unresolvable, information (e.g. scatterer size, dispersion, index of refraction, etc.) Such information could improve the diagnostic capabilities of OCT and result in better and earlier cancer diagnosis leading to improved prognosis and survival.
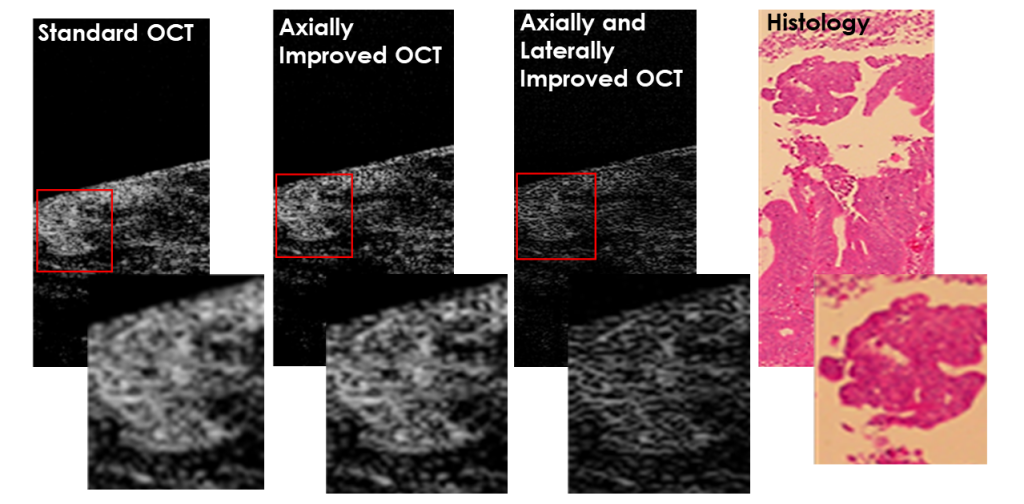
Resolution Improvement
The axial (depth) resolution of OCT depends on the spectral bandwidth of the source used. The lateral Resolution of OCT depends on the focal properties of the delivery optics. Current techniques to improve the resolution are limited by aberrations and the need for special hardware, which increase the complexity and cost and limit the scanning speed. In addition, the overall improvement is usually only a factor of two only when using deconvolution techniques. The ODx Lab has develop techniques to improve both the axial and lateral resolution of OCT using oversampling techniques with lead to a factor of 4-7x improvement.
Scatterer Size Estimation
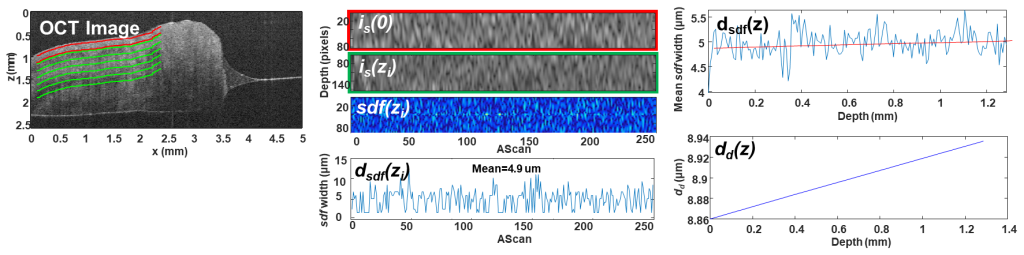
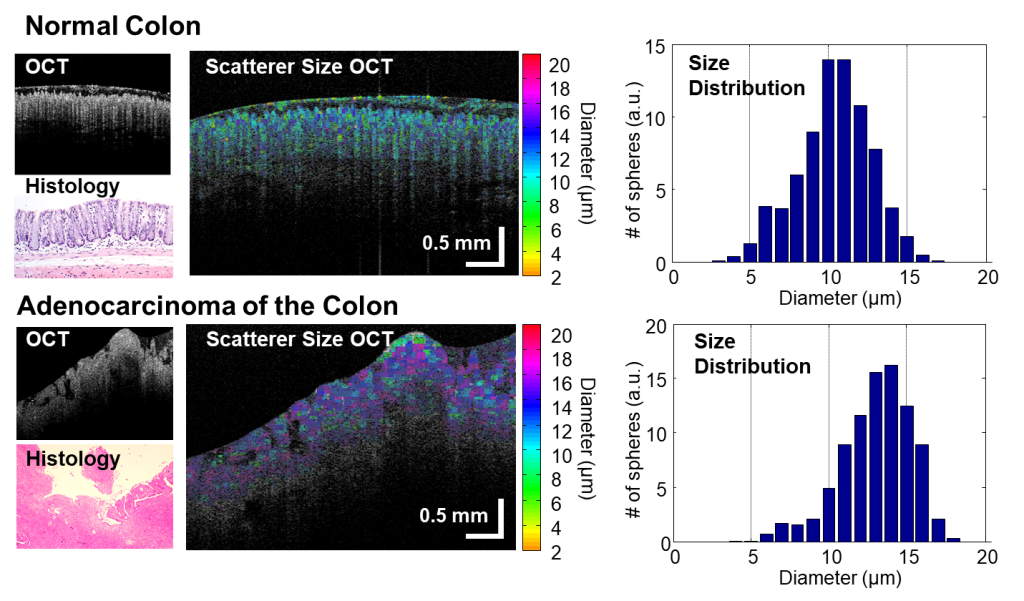
Variations in the size and density of cellular organelles are below the resolution limit of OCT and, therefore, cannot be resolved. However, they affect the spectrum of the back-reflected light and this effect can be seen when performing spectroscopic OCT imaging. The ODx Lab has developed a new metric to accurately and robustly determine the size of scatterers using spectroscopic analysis of the OCT signals. The process involves extracting the spectrum of the backreflected light and using the bandwidth of the correlation of the derivative to determine the scatterer size. Preliminary results show that the technique is sensitive enough to “see” differences between normal and abnormal tissues.
Dispersion Measurement
In OCT, dispersion mismatches cause degradation of the image resolution. However, dispersion is specific to the material that is causing the effect and can therefore carry useful information regarding the composition of the samples. In the ODx Lab, we have developed a novel technique for estimating the dispersion in tissue which uses the image speckle to calculate the PSF degradation and is therefore applicable to any tissue and can be implemented in vivo and in situ. The applicability to cancer diagnosis was evaluated on gastrointestinal normal and cancer OCT images. Using the statistics of the GVD estimate, the tissue classification resulted in 93% sensitivity and 73% specificity (84% correct classification rate).